
Continuous quality improvement (CQI) analyzes patient care to provide better, more efficient healthcare. This article provides expert guidance on the processes and models that healthcare organizations use to ensure quality improvement.
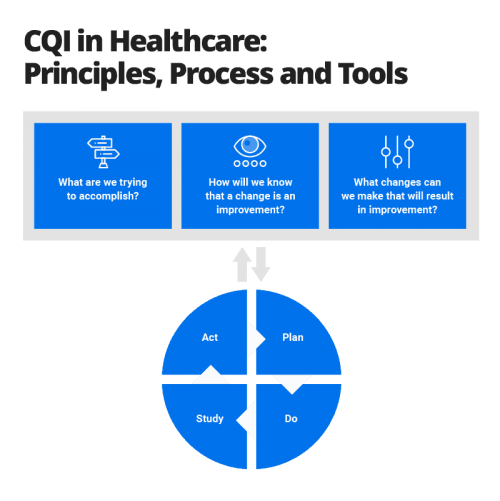
Continuous Quality Improvement (CQI) in healthcare an ongoing process of identifying, analyzing, and improving patient care outcomes and organizational performance. It involves a structured approach to problem-solving, data collection, and analysis to implement changes and enhance the quality of care.
A number of established models can help organizations perform effective continuous quality improvement. Many of those models originated and are still used in other industries. But they can apply to healthcare organizations. CQI models include the following:

Versions of some of these models focus on healthcare improvement, including the following:
A continuous quality improvement program often seeks to look more closely at a wide range of processes within a healthcare organization. But a CQI program also focuses on a specific aspect of an organization’s operation. One way to differentiate that focus is to categorize a program as either a CQI process study or a CQI outcomes study.
There are other methods of differentiating CQI projects. For example, some CQI efforts focus on how an individual patient in a particular condition is treated; others focus on treatment for a group of patients. Individual-level programs and group programs are described below:
The best CQI programs operate as their name suggests — continuously. But some organizations may have financial limitations that affect how often they can conduct CQI projects. The National Commission on Correctional Healthcare, for example, recommends that correctional facilities have either basic or comprehensive CQI programs according to the size of the facility.
You can successfully apply — and get help from — technology used in healthcare for your continuous quality improvement efforts. This is the case with the electronic health record (EHR) that exists for every patient.
An EHR is, in essence, a patient’s “chart” that at one time existed only on paper. It includes information on all recorded aspects of a patient’s health and the healthcare they have received. Recent federal legislation recommended a national goal for the “meaningful use” of EHR technology. That means all medical providers should have easy access to a patient’s EHR and use it to improve healthcare for all patients.
Organizations with a good CQI program can use their EHR information to gain a better understanding of the health of their patients, how certain care helped or hindered their well-being, and how to improve overall healthcare.
Continuous quality improvement in healthcare is an ongoing process to advance healthcare by always asking “How are we doing?” and “Can we do it better?” The goal is to improve healthcare by identifying problems, implementing changes to fix those problems, monitoring whether the changes help, and making further adjustments if they aren’t getting the desired results.
You might hear other terms in reference to CQI or to programs that are similar to CQI. They include the following:
Leading organizations involved with assessing healthcare quality have created standards and guidelines to understand what constitutes good healthcare quality and how healthcare can be improved. Here are two important sets of guidelines:
Continuous quality improvement in healthcare is a version of similar processes that began in manufacturing and can be traced back to the 1920s. Some healthcare leaders and academics began thinking more about healthcare quality improvement in the 1960s.
CQI processes were developed further in manufacturing in the 1970s and 1980s, as well as in healthcare in the 1990s. Here are some landmark times and important people in the development of CQI in healthcare.

Read more about “To Err Is Human” and “Crossing the Quality Chasm” in “A Business Guide to Effective Quality Improvement in Healthcare.”
Early academic analyses of the CQI movement in healthcare in the late 1990s found that, while the campaign had gained influence, it had yet to show many tangible results.
An 1998 academic study entitled “Assessing the Impact of Continuous Quality Improvement on Clinical Practice” was published in the Milbank Quarterly, a healthcare policy journal. The study authors analyzed 55 continuous quality improvement programs that had been studied and published in academic papers: 42 CQI programs at single sites and 13 CQI programs across multiple sites. They found that the outcomes of care had improved in a number of the cases.
“Particularly important correlates of success appear to be the participation of a nucleus of physicians, feedback to individual practitioners, and a supportive organizational culture for maintaining the gains that are achieved,” the authors wrote.
The authors warned, however, that the success of any new CQI program couldn’t be assumed from the results of the 55 cases. The CQI programs detailed as part of academic studies might have been more likely to succeed, the authors wrote. They couldn’t guess at the number of unsuccessful CQI programs that had never been outlined in academic papers, they wrote.
Another 1998 academic study — “A Report Card on Continuous Quality Improvement,” also published in the Milbank Quarterly — highlighted the progress to that point and the challenges of CQI.
Since 1998, CQI has been much more ingrained in the healthcare system and has produced consistently positive results. However, some of the recommendations and lessons detailed in the 1998 “report card” are still important today, including the following:
To learn more primary methods that can help you perform CQI — including Lean, Six Sigma, and others — along with the appropriate organizational foundation for CQI, tips for successful implementation, and the benefits of CQI to healthcare organizations’ operations, see “A Business Guide to Effective Quality Improvement in Healthcare.”
CQI academic researchers have pointed out that applying CQI to clinical practice usually involves three broad categories of problems:
You may encounter barriers and challenges with CQI programs, of course. Some of those barriers are due to the inherent structure of healthcare organizations and the healthcare system in the United States. They include the following:

“I think when you’re talking about people’s lives, and you know you’ve always done X and it works well … you’re probably going to stick with that,” says Heather Larivee, a CQI expert and the CEO of Sparkflo, LLC., a business consultancy. “Healthcare is a high-risk environment. The devil you know is less scary than the one you don’t know,” Larivee adds.

Organizations “have to designate a person in a senior leadership position to be the champion for quality within the organization,” says Stephanie Sargent, Vice President of Product Development and Quality for SE Healthcare, a South Carolina healthcare analytics and quality improvement company. “And that person needs to be highly influential,” she emphasizes.

“Staff members look to leadership for direction. If there isn’t someone who’s a visible champion within the organization, then employees of that organization have no reason to feel that quality is important,” Sargent points out.Kimberly McAdams, a process improvement expert and Principal with Firefly Consulting, agrees: “We are always going to be more successful when we have a commitment from upper management to really embrace the tools and methodologies and the new way of approaching what we do.”
To learn more about other challenges to performing good continuous quality improvement, see “A Business Guide to Effective Quality Improvement in Healthcare.”
As healthcare organizations have pursued likely tens of thousands of CQI initiatives or more over the past decade, they’ve done the work in a wide range of clinical and other areas. CQI work has been performed in hospitals, blood banks, ambulatory palliative care departments, and correctional institution medical departments, among thousands of other places.
CQI work has also focused on the following:
You can learn more about specific examples of CQI efforts in “The Largest Roundup of Healthcare Improvement Examples and Projects.”
The Centers for Medicare and Medicaid (CMS) and the Agency for Healthcare Research and Quality began developing a patient survey in the early 2000s to assess care for patients admitted to hospitals. The survey was first used in 2006, and results were first publicly reported in 2008.
The survey is called the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). It is administered to patients after they’ve been discharged from a hospital and asks about their experiences at the facility, including the following factors:
Results of the survey play a small part in how medical facilities are reimbursed for care of Medicare and Medicaid patients. The results are also publicly available on an HCAHPS website for prospective patients to use in evaluating a hospital. For both reasons, the survey encourages facilities to play close attention to certain areas of patient care and patient satisfaction.
In some ways, a continuous quality improvement project is similar to scientific medical research on a problem. But the two processes are also very different. Here are some distinctions between continuous quality improvement and medical research:
| CQI Projects | Research Projects |
|---|---|
| A CQI project adjusts processes to improve patient care. | A research project tests a hypothesis to add to general medical knowledge on a subject. |
| A CQI project produces findings for a healthcare facility to improve its operations. | A research project adds to general medical knowledge far beyond the healthcare facility. |
| A CQI project uses evidence-based standards. | A research project often tests new methods or standards not yet backed by evidence. |
| A CQI project attempts to make changes that result in patient benefit. | A research project may produce knowledge that has no benefit to a specific patient. |
| A CQI project often follows a method or cycle, such as the PDSA. | A research project adheres to the study design and often includes randomization of patients who get a new treatment versus those who don’t. |
| A CQI project includes most people who participate in a process. | A research project often includes a part of a specific population, with various patients intentionally included or excluded. |
| A CQI project requires a Health Insurance Portability and Accountability Act release to use a patient’s individual health information. | A research project must identify how it protects a patient’s individual health information and requires specific written consent from any patient to be included in the study. |
| A CQI project might make changes in the process, depending on its findings. | A research project does not change its original protocol; results are analyzed only when the project is finished. |
| The results of a CQI project are not intended to be published in a scientific journal, although they may be. | The results of a research project are expected to be published in a journal or presented to the medical or scientific community. |
| A CQI project is typically paid for by the healthcare organization itself. | A research project might be funded by external agencies or organizations. |
Top leaders of the Thibodaux Regional Medical Center in Thibodaux, Louisiana, knew the medical center needed to continuously improve in order to do well.
Chief Executive Officer Greg Stock set up a steering committee that included physicians and other leaders to spearhead the organization’s work in quality improvement. The steering committee, in turn, identified other top physicians and clinical leaders to be part of the work.
The group successfully tackled a number of quality improvement projects, including one to lower the mortality rates of its patients with sepsis, an overwhelming reaction by the human body to infection. Sepsis is a medical emergency and can quickly lead to organ failure and death.
Thibodaux Regional Medical Center leaders estimate that its quality improvement program saves 16 patient lives per year from sepsis. To learn more about Thibodaux Regional Medical Center’s sepsis quality improvement program — and dozens of other quality improvement programs — check out “The Largest Roundup of Healthcare Improvement Examples and Projects.”
Thibodaux has received a number of awards for its commitment to quality improvement, including an Outstanding Achievement Award from the American College of Surgeons’ Commission on Cancer and an award for hospital of the year for clinical excellence in pulmonary disease and respiratory care.
It’s important that your quality improvement program maintains its momentum beyond the first weeks, when staff enthusiasm might be highest. Here are some important activities and principles to follow to support the program and continually move it forward:
To aid in quality improvement work, you can try a wide range of tools, including the following:
Empower your people to go above and beyond with a flexible platform designed to match the needs of your team — and adapt as those needs change.
The Smartsheet platform makes it easy to plan, capture, manage, and report on work from anywhere, helping your team be more effective and get more done. Report on key metrics and get real-time visibility into work as it happens with roll-up reports, dashboards, and automated workflows built to keep your team connected and informed.
When teams have clarity into the work getting done, there’s no telling how much more they can accomplish in the same amount of time. Try Smartsheet for free, today.